LITTLE ROCK -- The state Department of Human Services announced that 4,353 Arkansans were no longer eligible for Medicaid benefits because over the past three months they failed to comply with work requirements.
Another 43,655 people met the work requirement and will retain their health coverage under Medicaid.
The news was the latest development in the long-running political struggle over the extent to which Arkansas should expand Medicaid, as required by federal mandates.
The federal law was enacted in 2010. It took several years and a number of lawsuits for the 50 states to implement its provisions.
Arkansas took a unique approach by making private health providers an integral part of the expanded Medicaid program. Lawmakers have adjusted our version of the health care act in each legislative session since the federal mandate was imposed. Currently, the program is known as Arkansas Works and it requires enrollees to either work, consistently look for work or attend classes that will teach job skills.
Two state agencies were present when the announcement was made -- the Human Services Department because it administers Medicaid, and the Workforce Services Department because it provides the job hunting services required of enrollees.
For three months the 4,353 people who were removed from the Medicaid rolls failed to report their attendance at class, or their job schedules or any volunteer work that would have brought them in compliance.
Department officials announced that more than 5,000 people are in jeopardy of losing their benefits at the end of September because they have gone two months without complying with the work requirements.
Critics say that the requirements place too much of a burden on Medicaid recipients. For example, many recipients probably don't have a computer, a smart phone or Internet access that is necessary to meet the requirements.
DHS officials defended their efforts to notify recipients of the requirements, and to help them respond. They sent 136,000 letters and made more than 150,000 phone calls. They sent text messages and in some cases visited people's houses. They conducted training sessions and posted materials in doctors' offices and emergency rooms.
Recipients who lack Internet access could get help by calling their insurance carrier, or visiting a county DHS office for help.
The people who lost coverage will be ineligible until the end of 2018, but they might qualify in other categories of Medicaid if their circumstances worsen, or if they are pregnant or have a disability.
Currently, the work requirement applies to enrollees from 30 to 49 years of age. They must work 80 hours a month, or take vo-tech classes. Up to 39 hours a month can be spent looking for work or attending a job search training class at a local Arkansas Workforce Center. Up to 20 hours in a year can be spent taking health education classes. Each hour spent volunteering counts as an hour of work.
It's important to contact DHS when your economic circumstances change. In fact, it's a good idea to keep in contact with DHS when people move in or out of your house, if a family member is discharged from a nursing home, or if you decide to claim a child as a dependent.
•••
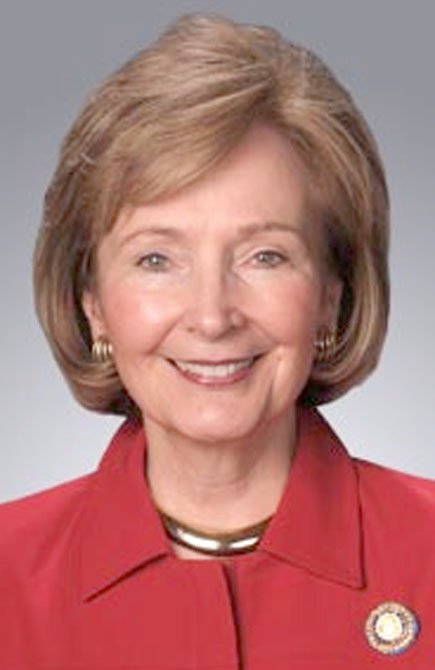
Editor's note: Arkansas Senator Cecile Bledsoe represents the third district. From Rogers, Sen. Bledsoe is chair of the Public Health, Welfare and Labor Committee.
Editorial on 09/19/2018